The central government has introduced the Pradhan Mantri Jan Arogya Yojana 2022, also known as Ayushman Bharat Yojana. The National Health Protection Scheme seeks to offer needy households up to Rs. 5 lakh in annual health insurance coverage. Around 100 million (10 crores) poor and BPL families (around 50 crore citizens) from all throughout the nation would be covered by the central government through the Ayushman Bharat Yojana.
For secondary and tertiary care hospitalization, the PM Jan Arogya Yojana or Ayushman Bharat Scheme would offer cashless and paperless treatment. The central and state governments will cover the full cost of implementing the plan, including the insurance premium. The central government has decided on the Ayushman Bharat Treatment Package Rates, which have been placed on the new NHPM Portal.
The Ayushman Bharat Yojana also includes the opening of 1.5 Lakh health and wellness centers nationwide to bring health services closer to people in addition to offering cashless insurance benefits. These health and wellness facilities will offer free access to basic diagnostic procedures and necessary medicines.
Ayushman Bharat Yojana Enrollment / Application / Registration
To receive the benefits of the Ayushman Bharat Yojana, there is no requirement for enrollment, application, or registration of any type. It is an eligibility-based program where the beneficiaries are chosen based on a number of factors, including the SECC-2011 data. By dialing the helpline number at 14555 or going to the official “Am I Eligible” portal at mera.pmjay.gov.in, one can determine whether they are eligible for the Ayushman Bharat Yojana.
There hasn’t been any official announcement regarding the Ayushman Bharat Yojana’s online registration or applications as of yet. However, Golden Cards are available to all beneficiaries whose names are listed on the PM Jan Arogya Yojana List. Beneficiaries of the Ayushman Bharat Yojana can now access PMJAY services through Common Service Centers (CSCs).
How to apply for Ayushman Bharat Yojana’s Online Application
For the Ayushman Bharat Yojana, there is no need to apply online or offline because it is an eligibility-based program. For the scheme, there are no online application forms or registration processes.
Selection of Ayushman Bharat Yojana Beneficiaries
Ayushman Bharat Yojana eligibility requirements are exclusively based on data from the Socio-Economic Caste Census (SECC), which covers both rural and urban areas nationwide. The entire number of beneficiary households, which includes impoverished rural families and families belonging to a specific occupational category of urban workers, will be around 10.74 crores.
However, if the criterion for inclusion/exclusion, deprivation/occupation, or both, in SECC data change in the future, the plan will take all changes into account, and beneficiary families will be included/excluded based on the same altered criteria. Additionally, see the
Coverage / Implementation of the Ayushman Bharat Yojana
All of the states and union territories shall execute the National Health Protection Initiative/Mission under the Ayushman Bharat scheme to provide coverage for all of the targeted beneficiary families throughout the nation. Under the direction of the Government of India’s Ministry of Health and Family Welfare, the Ayushman Bharat National Health Protection Mission Agency (AB-NHPMA) will carry out the initiative.
The State Health Agency (SHA), freshly founded or formed utilizing an existing trust, society, non-profit company, or state nodal agency, would be in charge of implementing the scheme in the relevant state and UT. The cashless advantages of treatment under the program will be accessible at all accredited private hospitals and government hospitals country, excluding those on the negative list.
Important Features of Ayushman Bharat Yojana
Here are some of the important features of the Ayushman Bharat Yojana:
- The two main projects launched under the Ayushman Bharat Scheme are the National Health Protection Mission and Health & Wellness Centers.
- For secondary and tertiary care hospitalization, the National Health Protection Mission would provide insurance coverage of up to Rs. 5 Lakh per family each year.
- In hospitals and other healthcare facilities around the nation, 1.5 lakh health and wellness centers would be established. More than 18 thousand are now in use.
- Over 10 crore impoverished rural and urban families—roughly 40% of the nation’s overall population—will receive health insurance coverage under the program.
- Beneficiaries will be chosen based on information from the SECC.
- The size of the covered beneficiary family will not be restricted.
- The scheme will improve overall patient satisfaction by ensuring that patients receive prompt care. Healthcare services will be more productive and efficient overall, which will raise everyone’s standard of living.
- The central and state governments, according to the ratio set by the Ministry of Finance, will pay the full cost of the insurance premium.
- The entity in charge of the scheme’s implementation in the states would be the State Health Agency (SHA).
- The government would specify the cost of the treatments in advance as a set price to keep costs under control.
- Benefits from the scheme would be portable across the nation, allowing beneficiaries to get cashless medical care at any government- or privately-owned hospital that is affiliated with the program.
- The central government would create a reliable, modular, scalable, and interoperable IT platform in partnership with NITI Aayog to facilitate paperless and cashless transactions.
- The current centrally sponsored programs Rashtriya Swasthya Bima Yojana (RSBY) and the Senior Citizen Health Insurance Scheme will be absorbed into Ayushman Bharat – National Health Protection Mission (SCHIS).
View the full Ayushman Bharat Yojana (PMJAY) Claim Settlement Guidelines in the section below.
Information & Quick Facts about Ayushman Bharat
| Data Point | Fact / Information |
|---|---|
| Name of Scheme / Initiative | Ayushman Bharat Scheme |
| Announced | 1 February 2018 by Prime Minister Narendra Modi |
| Launched | 23 September 2018 |
| Initiatives Under the Scheme | 1. National Health Protection Mission 2. Health & Wellness Centers |
| Implementing Authority | Ayushman Bharat National Health Protection Mission Agency (AB-NHPMA) under Ministry of Health and Family Welfare, Government of India |
| Scheme Coverage | All states and Union Territories |
| Budget Allocation | Rs. 6400 Crore in 2021-22 Union Budget |
| No. of Beneficiaries in NHPM | More than 10 Crore Families Under National Health Protection Mission Initiative |
| Benefits of NHPM | Health insurance coverage of up to Rs. 5 Lakh per annum per family for secondary & tertiary care hospitalization |
| Selection of Beneficiaries in NHPM | Deprived rural & identified occupational category of urban workers’ families as per SECC-2011 data |
| Size of covered beneficiary family in NHPM | No restriction on family size |
| Insurance premium for NHPM | Entire cost of premium to be borne by central & state governments |
| Treatment availability in NHPM | At all government & empaneled private hospitals |
| What is Health & Wellness Center | Health & wellness centers to provide basic health services / diagnostics & basic drugs for free. |
| Facilities at HWCs | Point of care for diagnostics / hub & spoke, wellness rooms for Yoga, Physiotherapy & group meetings, separate consulting space, free drug dispensation, telemedicine facilities, storage space for drugs & consumables and waiting area for 30+ people |
| No. of Health & Wellness centers | 1.5 Lakh total number to be started till December 2022 |
| Beneficiaries | All citizens of the country |
| More details | Ayushman Bharat Health & Wellness Centers |
Ayushman Bharat Yojana Overview
On the official website, pmjay.gov.in, you may find more information about the Ayushman Bharat – National Health Protection Mission, including a list of hospitals and a list of beneficiaries.
About Pradhan Mantri Arogya Jana Yojana (PMJAY)
On September 23, 2018, Prime Minister Narendra Modi introduced the Pradhan Mantri Jan Arogya Yojana (PMJAY). A mega National Health Protection Scheme (NHPS) for the poor, the PMJAY Scheme. For secondary and tertiary hospitalization, PMJAY would offer health insurance worth Rs. 5 Lakh. About 50 crore poor individuals will receive cashless and paperless hospital care thanks to the Ayushman Bharat Yojana.
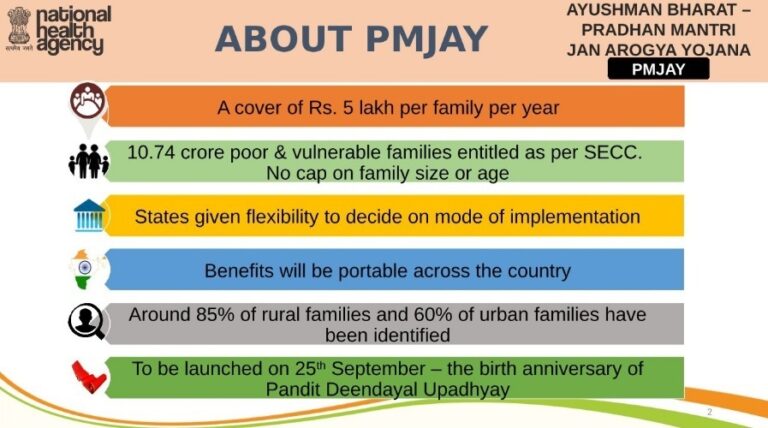
To receive PMJAY benefits, people can go to any Health and Wellness Center. Ayushman Family Cards would be sent to all AB-NHPM beneficiaries, and Arogya Mitras will receive assistance training. Visit this page for a detailed explanation of the PMJAY Scheme. The following are Pradhan Mantri Jan Arogya Yojana’s key characteristics and highlights:-
- A family’s annual health insurance coverage is Rs. 5 lakh.
- Eligible families are the 10.74 crore poor and vulnerable families whose names appear in the SECC-2011 Data. Age and family size are not restricted.
- The mode of implementation is left up to the states’ discretion.
- Benefits will be transferable throughout the country.
- The identities of about 85% of rural households and 60% of urban families are known.
- Released on September 25, 2018, the anniversary of Pandit Deendayal Upadhyay’s birth.
 About Pradhan Mantri Jan Arogya Yojana PMJAY
About Pradhan Mantri Jan Arogya Yojana PMJAY
Important Steps in the Implementation of PMJAY
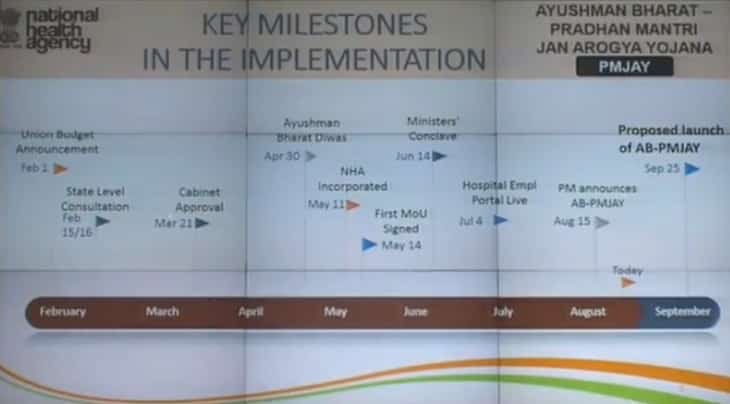
The following list of important PMJAY Implementation milestones is provided to you: – — It was declared in the Union Budget 2018 on February 1st.
— A State Level Consultation took place on February 15 and 16, 2018.
— On March 21, 2018, the Cabinet approved the Ayushman Bharat Yojana.
— 30 April 2018 (Ayushman Bharat Diwas – Starting Date of Beneficiary Identification).
— On May 11, 2018, the National Health Agency (NHA) was established.
— On May 14, 2018, the first Memorandum of Understanding was signed.
— The Ministers Conclave was held on June 14, 2018.
— On July 4, 2018, the Hospital Empanelment Portal went live.
— On August 15, 2018, the Pradhan Mantri Jan Arogya Yojana (PMJAY) announcement was made.
— On September 25, 2018, the Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana launched.
 Important Steps in the Implementation of PMJAY
Important Steps in the Implementation of PMJAY
Modes of Implementation for AB-PMJAY
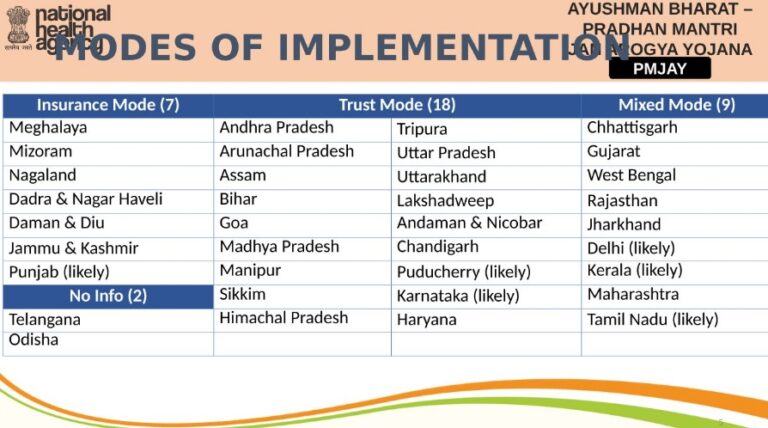
This Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana can be implemented in whatever way the state chooses (AB-PMJAY). Three modes exist: the Insurance Mode, the Trust Mode, and the Mixed Mode. Below is a list of the states’ names and their chosen PMJAY manner of implementation.
 Modes of Implementation for AB-PMJAY
Modes of Implementation for AB-PMJAY
Seven states have chosen to implement this AB-PMJAY Scheme in Insurance Mode, 18 in Trust Mode, 9 in Mixed Mode, and 2 states have not yet made a decision.
Restrictive Actions Against Fake PMJAY Websites
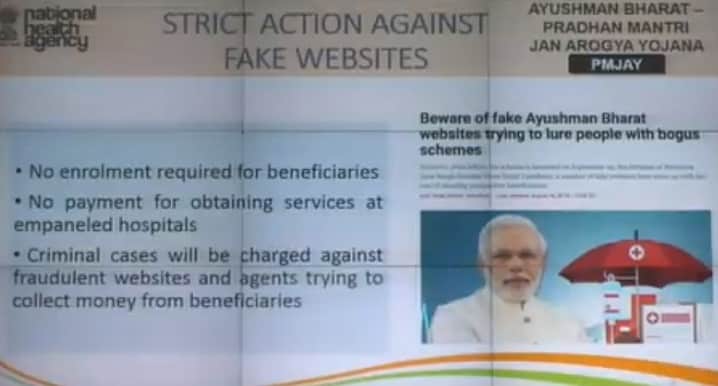
Regarding Ayushman Bharat – PMJAY, everyone should be aware of the following:
- Beneficiaries can use the National Health Protection Scheme’s benefits without enrolling.
- In order to receive services at hospitals with an appointment, he or she cannot pay anything.
- Criminal charges will be brought against websites and agents that attempt to defraud beneficiaries of their money.
 Restrictive Actions Against Fake PMJAY Websites
Restrictive Actions Against Fake PMJAY Websites
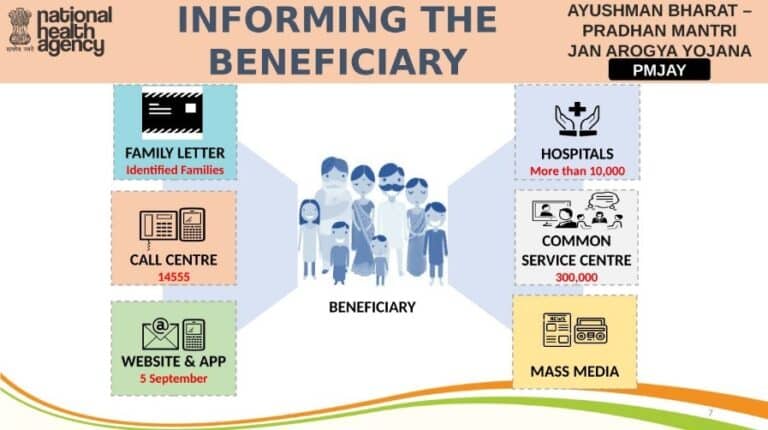
The Pradhan Mantri Jan Arogya Yojana Beneficiaries Being Informed
The following details the full Pradhan Mantri Jan Arogya Yojana Beneficiaries notification process:
- Families who have been identified will get family letters.
- For those who are Pradhan Mantri Jan Arogya Yojana beneficiaries, call centre “14555” would be available.
- The websites and apps went live on September 5, 2018.
- People can get information on Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana is available through 10,000 hospitals, 3 lakh CSCs, and the media.
 The Pradhan Mantri Jan Arogya Yojana Beneficiaries Being Informed
The Pradhan Mantri Jan Arogya Yojana Beneficiaries Being Informed
At mera.pmjay.gov.in, candidates can also check their names on the list of PM Jan Arogya Yojana recipients.
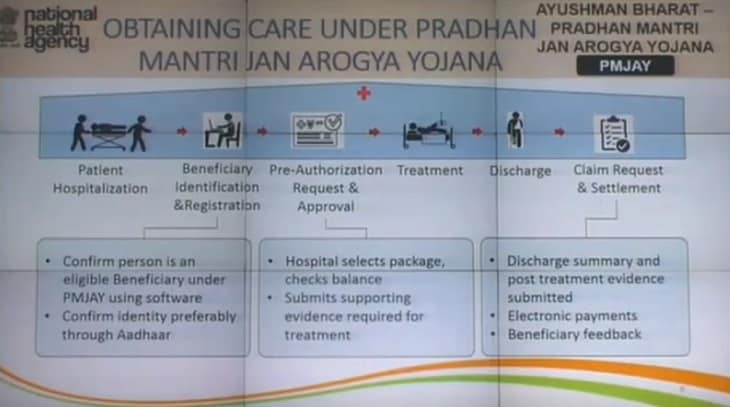
Receiving Medical Care under Pradhan Mantri Arogya Yojana, Jan
To receive care through the Pradhan Mantri Jan Arogya Yojana, the following steps must be taken:
Patient Hospitalization – First, patients must be admitted to hospitals.
Beneficiary Identification & Registration: This process uses software to determine whether a person is a PMJAY beneficiary. Additionally, identity verification, preferably through Aadhaar.
Pre-Authorization Request & Approval – Hospitals will choose the package and check the card’s balance. They will then submit the supporting documentation required for treatment.
The patient would then receive the proper treatment.
Discharge – Patients would receive a discharge after receiving the proper care.
Evidence from the post-treatment period as well as the claim request and settlement would be provided. The government would pay the banks electronically. Hospitals will ask patients for comments once they have received therapy.
 Obtaining Care Pradhan Mantri Jan Arogya Yojana
Obtaining Care Pradhan Mantri Jan Arogya Yojana
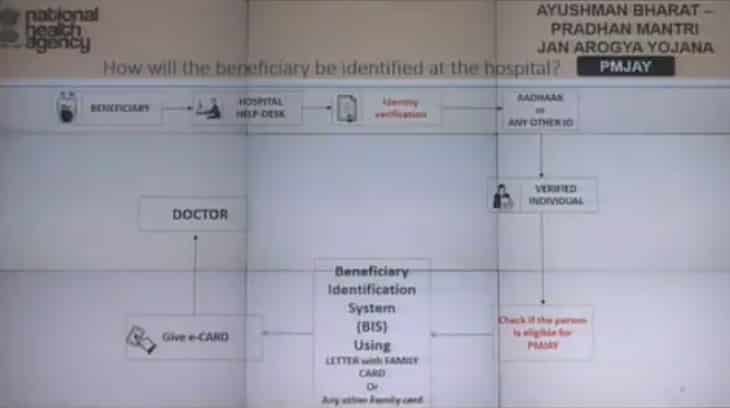
How will the Ayushman Bharat-PMJAY Beneficiary be Recognized at the Hospital?
The beneficiary must first visit the hospital help desk where identity verification must be completed. An Aadhaar Card or another form of ID must be shown for this. The person will then be confirmed and his or her eligibility will be determined. A beneficiary identification system (BIS) using a letter and family card is used for this. The beneficiaries will then be handed an electronic card to present to their doctor for treatment.
 Ayushman Bharat PMJAY Beneficiary Identification Hospital
Ayushman Bharat PMJAY Beneficiary Identification Hospital
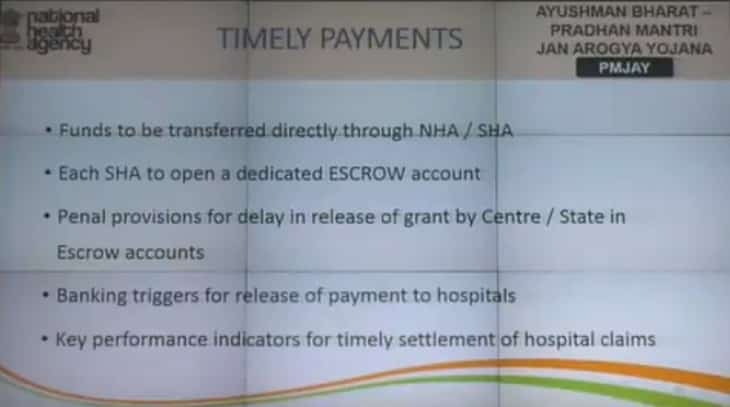
Ayushman Bharat – Pradhan Mantri: Timely Payments of Jan Arogya Yojana
Payments for medical care will be made on time to all hospitals. On-time payments are promised and will be made in the following ways:-
- Direct transfers of funds will be made through the State Health Agency or National Health Agency (NHA) (SHA).
- Each SHA must set up its own ESCROW account.
- In ESCROW Accounts, there are sanctions for the Center’s or State’s delayed release of grants.
- Payments to hospitals are released as a result of banking events.
- Key performance indicators for a prompt hospital claim payout.
 Ayushman Bharat – Pradhan Mantri: Timely Payments of Jan Arogya Yojana
Ayushman Bharat – Pradhan Mantri: Timely Payments of Jan Arogya Yojana
Anti-Fraud Guidelines for the AB-Pradhan Mantri Jan Arogya Yojana
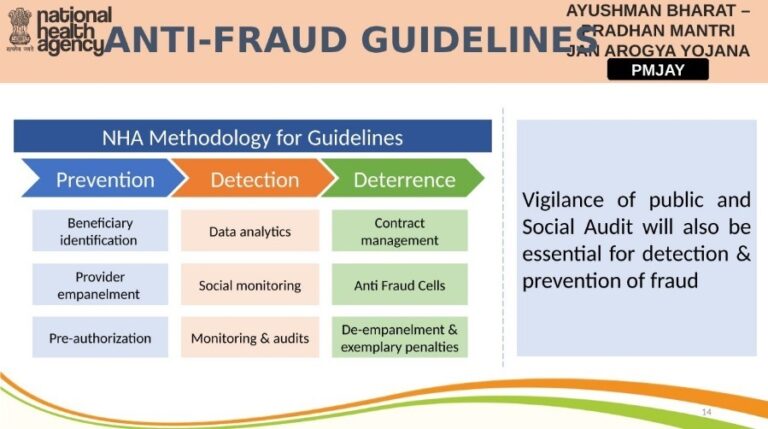
The NHA Methodology for Guidelines has just been released. This covers Prevention, Detection, and Deterrence. Beneficiary Empanelment, Pre-Authorization, and Provider Identification are all components of prevention. Data analytics, social media monitoring, audits, and other detection methods will be used. Contract management, anti-fraud cells, de-empanelment, and exemplary penalties are all forms of deterrence.
 Anti-Fraud Guidelines for the AB-Pradhan Mantri Jan Arogya Yojana
Anti-Fraud Guidelines for the AB-Pradhan Mantri Jan Arogya Yojana
Public and social audit vigilance will also be required for the detection and prevention of fraud.
NHA Data Privacy & Information Security Policy
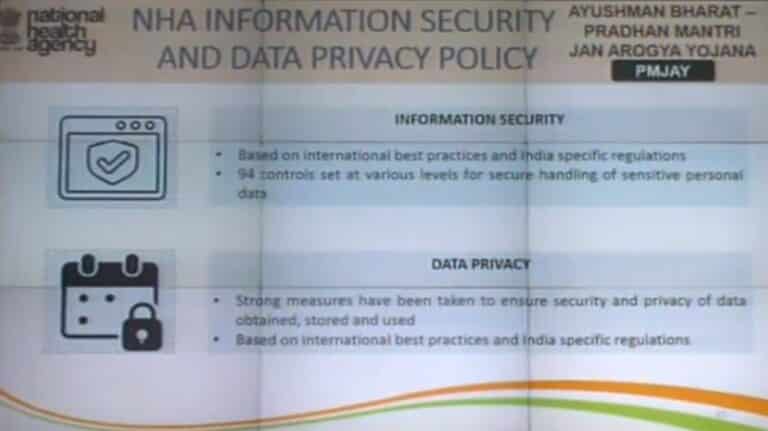
India-specific regulations and international best practises would serve as the foundation for the information policy. For the secure processing of sensitive personal data, 94 controls are set at various levels. For the purpose of obtaining, storing, and using data privacy, serious measures have been implemented. Based on international best practises and laws relevant to India.
PMJAY Package Rates for Pradhan Mantri Jan Arogya Yojana
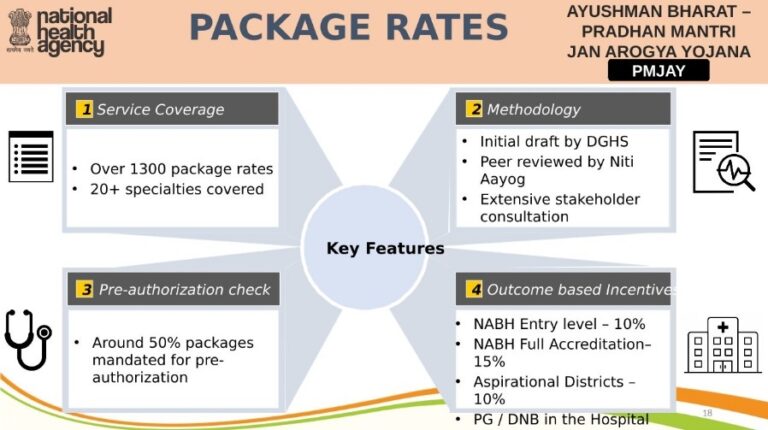
20+ specialties have been covered, and around 1300 packages have been authorized. NITI Aayog peer examined the DGHS’ initial draught after considerable stakeholder input. About 50% of packages are required to have pre-authorization. Hospitals can get outcome-based incentives, such as 10% rewards for NABH Entry Hospitals, 15% incentives for NABH Full Accreditation, and 10% incentives for Aspirational Districts.
 PMJAY Package Rates for Pradhan Mantri Jan Arogya Yojana
PMJAY Package Rates for Pradhan Mantri Jan Arogya Yojana
PMAM Training (Pradhan Mantri Arogya Mitra)
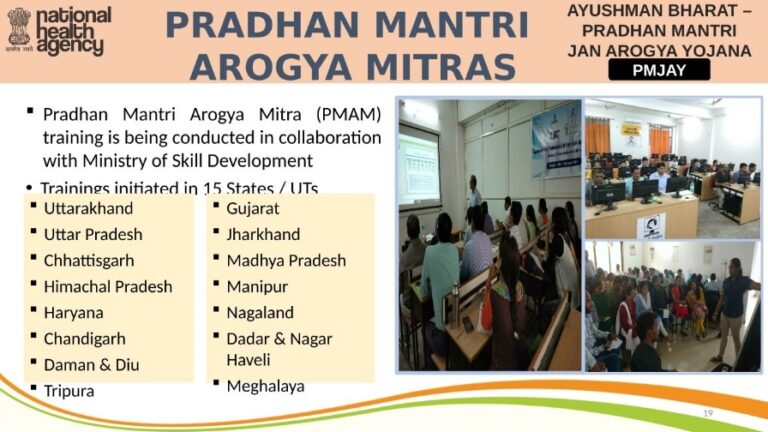
The Ministry of Skill Development and Pradhan Mantri Arogya Mitra (PMAM) are working together to conduct training. In 15 States and UTs, training has already begun.
 PMAM Training (Pradhan Mantri Arogya Mitra)
PMAM Training (Pradhan Mantri Arogya Mitra)
Launch of PM Jan Arogya Yojana
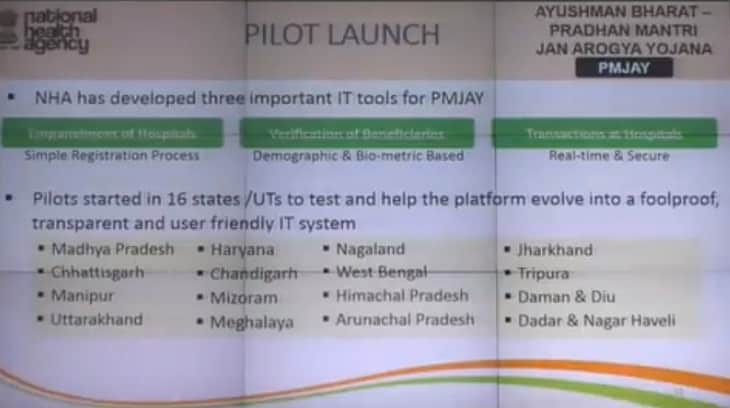
For PMJAY, the National Health Agency (NHA) has created three crucial IT tools. These include the simple registration process for hospital empanelment, beneficiary verification based on demographic and biometric data, and real-time, secure transactions at hospitals. A pilot project was launched in 16 States and UTs to test the platform and aid in its evolution into a secure, open, and user-friendly IT system.
 Launch of PM Jan Arogya Yojana
Launch of PM Jan Arogya Yojana
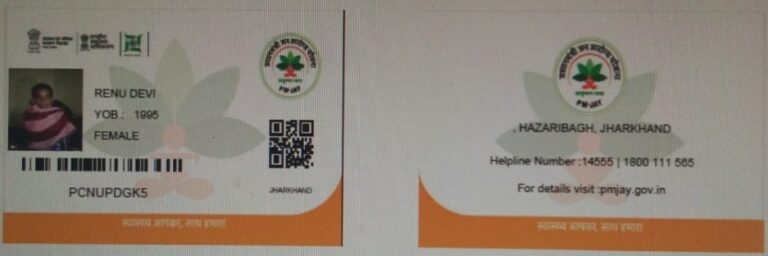
Ayushman Bharat Golden Cards – PM Jan Arogya Yojana Golden Cards
Beneficiaries are eligible for Golden Cards so they can receive care in any government- or privately-impaneled hospital. Following is how this golden card will show up:-
 PM Jan Arogya Yojana Golden Cards
PM Jan Arogya Yojana Golden Cards
3 days before and 15 days after a hospital stay, the government’s ambitious Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana would cover medications and diagnostic fees for poor and vulnerable families up to Rs 5 lakh in hospitalization expenditures.
Current Updates on Ayushman Bharat Yojana (Date Wise)
Here are all of the most recent Ayushman Bharat Yojana updates, organized by date. As of the updated date, the language used in the writing is:
Online Application for Hospital Empanelment under the Ayushman Bharat Scheme (Update on 11 April 2020)
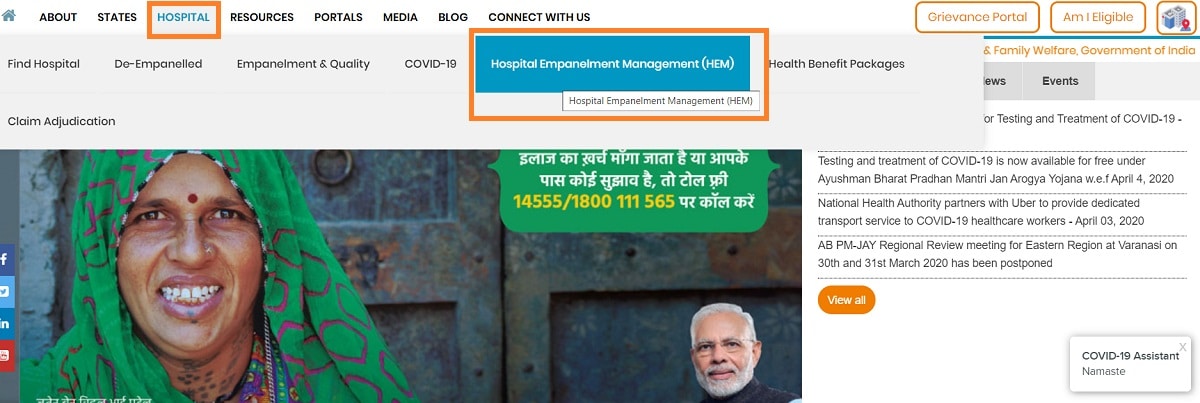
The Ayushman Bharat Yojana is currently accepting online applications for hospital empanelment. All private hospitals have now started the official express process to appoint hospitals through registration to handle COVID-19 (Coronavirus). Any hospital can enroll in the Prime Minister Rashtriya Swasthya Suraksha Mission (PMRSSM) by completing the Hospital Empanelment Online Application Form at pmjay.gov.in.
The Pradhan Mantri 10.74 crore poor and underprivileged rural people would receive health protection through the Jan Arogya Yojana (PMJAY). With no limitations on age, family size, or gender, the government would offer cashless and paperless benefits of up to Rs. 5 lakh to low-income patients in any government- or privately-empanelled hospital under the Modicare scheme.
For a list of hospitals covered by the Pradhan Mantri Jan Arogya Yojana, search under Ayushman Bharat. People can only get health benefits through a single prescribed ID, and there are no prerequisites for treatment. The government believes that as a person’s economic background is irrelevant to their health, neither should their treatment.
Application for Ayushman Bharat Scheme’s PMJAY Hospital Empanelment
The steps in detail for hospitals to complete the National Health Protection Scheme (NHPS) Hospital Empanelment Online Application Form are provided below:-
- First, go to PMJAY.gov.in, the official website.
- Click the “Hospital” tab, followed by the “Hospital Empanelment Management (HEM)” tab, as shown in the image, on the portal.
 Application for Ayushman Bharat Scheme’s PMJAY Hospital Empanelment
Application for Ayushman Bharat Scheme’s PMJAY Hospital Empanelment
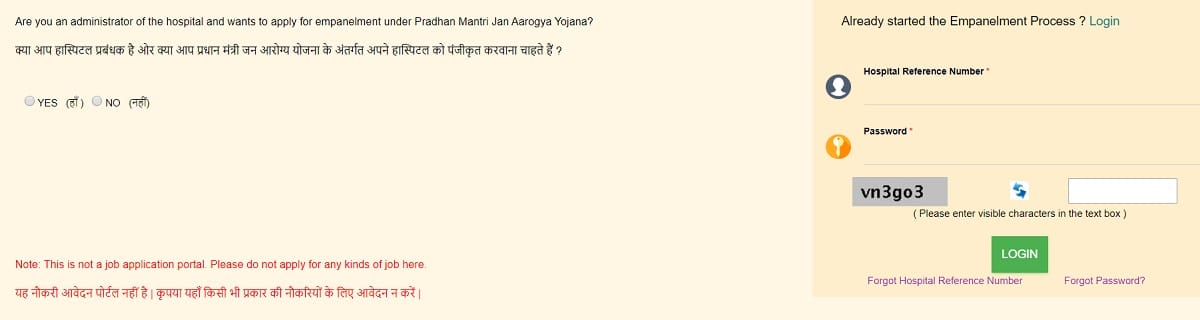
- Direct Link for PMJAY Hospital Empanelment under the Ayushman Bharat Scheme – https://hospitals.pmjay.gov.in/empApplicationHome.htm?actionVal=loginPage
- The Hospital Empanelment Module (HEM) lite page for express empanellment of private hospitals will soon launch.
 PMJAY Express Private Hospital Empanelment
PMJAY Express Private Hospital Empanelment
- The Ayushman Bharat Yojana Hospital Empanelment Online Application Form will appear as follows:
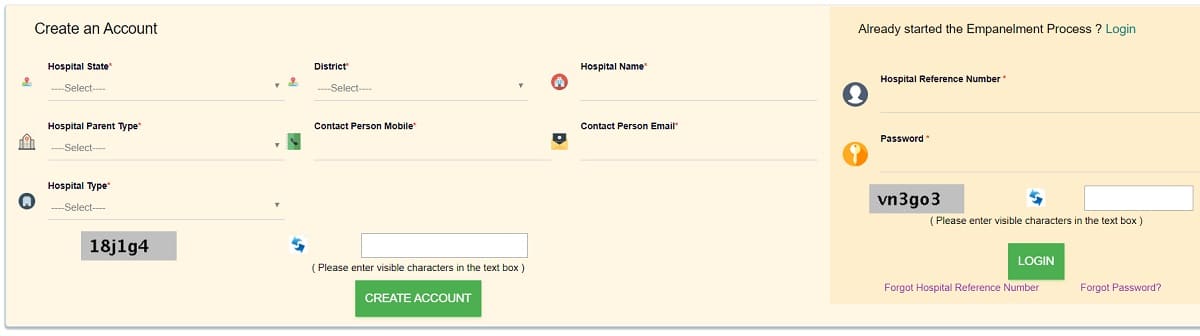 Ayushman Bharat PMJAY Hospital Empanelment Online Application Form
Ayushman Bharat PMJAY Hospital Empanelment Online Application Form
- To complete the hospital empanelment process, hospitals can enter the state, name of the hospital, hospital parent (single or group), contact person’s email address, password, and hospital type (public, private (not for profit), or private (profit)) here. Then, they can click the “Create an Account” button.
Before registering and logging in, hospitals must also review the empanelment requirements. Hospitals that are RSBY-empaneled do not need to register again. The RSBY hospital code that is printed on your MHC can be used by hospitals to create “Login” pages. The password can be the hospital’s PIN code.
Benefits of the Ayushman Bharat Yojana
The beneficiaries of the new National Health Protection Scheme will receive the following benefits:-
- 5 lakhs in insurance coverage per family, per year.
- There are no limitations on family size, age, or gender.
- The SECC Database/Ayushman Bharat Yojana Rural & Urban List of Beneficiaries contains the names of all Eligible Family Members; these individuals are automatically covered.
- In the event of hospitalization, beneficiaries are not required to pay any money for the treatment.
- Existing conditions will be covered starting on the first day of the insurance. Pre- and post-hospitalization procedures are also included in these advantages.
- Any public, private, or private empaneled hospital can treat patients.
- To receive medical care at the hospital, people must have a prescribed ID with them.
For assistance with the Hospital Empanelment Query, contact +918860003730 during working time.
Empanelment under the Ayushman Bharat Yojana of NHA Express Private Hospital
Express empanelment is started by the National Health Authority (NHA) to bring a large number of private hospitals under the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB-PMJAY). This empanelment of private hospitals would guarantee ongoing, crucial care for critical illnesses including cancer and heart conditions. This decision was made in response to a recent one that included COVID-19 testing and treatment inside the AB-PMJAY plan. According to the ICMR’s policies and recommendations, coronavirus will be treated.
A number of medical colleges, civil hospitals, and district hospitals are being transformed into special COVID-19 facilities in the current Novel Coronavirus (COVID-19) outbreak. For patients with critical illnesses like cancer, cardiac problems, and diabetes, the Hospital Empanelment Module (HEM) Lite has been introduced. All of these patients need ongoing care and can continue receiving inpatient care without worrying about obtaining a COVID-19 infection.
This quick process for adding private hospitals to the Ayushman Bharat Yojana system would also aid in adding COVID-19 hospitals. Through a more straightforward, user-friendly online mechanism accessible on the scheme website www.pmjay.gov.in, hospitals can impanel themselves for a temporary duration of 3 months.
Treatment For Serious Illnesses in Ayushman Bharat PM-JAY
As many currently impanelled hospitals transform themselves into dedicated COVID-19-only facilities, care for AB-PMJAY patients must not suffer. The central government has begun express empanelment of private hospitals on a temporary basis in order to strengthen our capacity to serve participants of the PMJAY Scheme. The government is contacting states, hospital groups, and organizations representing the healthcare sector with this new idea. The new method will temporarily onboard private hospitals using a straightforward, efficient, and seamless system.
All of these hospitals have the option to opt-out of the program’s regular treatment of critical illnesses like cancer and cardiac conditions. Additionally, these institutions have the option to become COVID-19-only facilities, offering specialized testing and care to COVID-19 patients.
Timeline of PMJAY Hospital Empanelment on HEM Lite
A hospital can complete the application form and attach supporting documentation in less than an hour using the HEM Lite. The Hospital Empanelment Management (HEM) system is designed to make sure that the procedure for approval by the relevant authorities is quick. A manual for empanelment has also been supplied for your convenience. If hospitals run into trouble, they can call the NHA representative for a quick resolution and complete assistance with submitting the paperwork.
Hospitals are compensated at pre-fixed rates under the scheme, which includes more than 1500 health benefits packages for secondary and tertiary care operations. Periodically, the package pricing is changed, and new rates were introduced in 2016. In addition to the indicated price, hospitals may receive additional incentives totaling up to 39% (cumulative) for NABH entry-level/full accreditation, geographic location (metro/aspirational areas), and for offering PG courses.
Currently, there are 96 lakh hospitalizations at more than 8,804 private hospitals across the country that are empaneled with the AB PM-JAY scheme, accounting for 51% of all treatments, and 64% of hospital admissions (Rs 13,000 crore). There is a strong mechanism in place for handling complaints, and the claim money is given within 15 days of the hospital submitting the proper documents.
Treatment and testing for the novel coronavirus (COVID-19) are free under the Ayushman Bharat (PMJAY) Scheme (Update on 4 April 2020)
Under the Ayushman Bharat Scheme 2020, the central government has begun providing free treatment and testing for novel coronavirus symptoms. People can now go for free checks if they exhibit symptoms like pneumonia, fever, or difficulty breathing. The PM Jan Arogyua Yojana will also offer the full COVID-19 treatment to the sick person. Beneficiaries can continue to receive this free treatment for coronavirus disease symptoms through various Ayushman Bharat PMJAY packages.
All COVID-19 disease patients can now make use of free treatment, testing, and checkup services at private labs, governmental hospitals, empanelled private hospitals, and other designated hospitals. The National Health Authority (NHA) will serve as the nodal organization for treating COVID-19-infected individuals. More than 50 crore individuals would now qualify for COVID-19 testing and treatment through the Ayushman Bharat Health Insurance scheme.
Call the state helpline number or the federal government control room at 011-23978046 if you have a fever, cough, or difficulty breathing.
Ayushman Bharat Yojana provides free coronavirus (COVID-19) treatment and testing
Pneumonia, fever, and respiratory failure are among the conditions for which Ayushman Bharat-PMJAY provides free medical care. In public facilities, COVID-19 testing and treatment are already free. More than 50 crore citizens who qualify for the health assurance scheme will now be able to obtain free COVID-19 treatment at accredited hospitals as well as testing through private labs. Treatment of #COVID19 #Corona symptoms like pneumonia, fever, respiratory failure, etc. is available, through various packages, under #AyushmanBharat #PMJAY free of charge for eligible people in empanelled hospitals & other designated hospitals, according to a tweet from a central government official.
Ayushman Bharat PM Jan Arogya Yojana (AB-PMJAY), the central government’s flagship Yojana, provides insurance coverage of up to Rs. 5 lakh per household every year. More than 10.74 crore poor and vulnerable families nationwide can use this health insurance facility for secondary and tertiary care hospitalisation. All AB-PMJAY beneficiaries have the right to obtain hand rub services at approved hospitals without having to use cash or paper.
Over 20,761 public and private hospitals across the nation have been empanelled, and there are currently 1,578 health benefits packages with defined prices under PM-JAY. See the prices for Ayushman Bharat Yojana. The central government has currently distributed 12.41 crore e-cards to AB-PMJAY recipients. Additionally, 91.70 lakh hospital admissions reportedly occurred under the scheme, according to NHA.
The Indian Council for Medical Research (ICMR) will approve or register private laboratories to perform the COVID-19 tests in accordance with its procedures. According to medical professionals, the two most effective methods for combating the extremely contagious Coronavirus are social isolation and thorough testing. Over a million people worldwide have been affected by the COVID-19 virus. While the national lockdown is being carefully enforced by the center to stop the virus’s spread, the country has one of the lowest rates of testing among the impacted countries.
The center has recruited a number of private labs to increase the number of coronavirus testing sites. However, because they are expensive—Rs 4,500 for each test—there have been worries that the impoverished won’t be able to buy them. If the number of COVID-19 patients who require care increases, active private-sector involvement will be essential. The NHA noted that states are working to register hospitals in the private sector that can become COVID-19 ONLY facilities.
Precautions Against a Novel Coronavirus (COVID 19)
Now, people can protect themselves from coronavirus by doing the following:
- Wash your hands frequently with soap and water.
- Use a hand cream with alcohol in it.
- Do not touch your lips, nose, or eyes.
- Maintain your distance from others.
- Stay away from organizing and joining big groups.
- When you cough and sneeze, cover your mouth.
- Avoid spitting in public.
- If you have a cough or fever, keep your distance.
Cases of coronavirus in India
By 4 April 2020, there would have been 2,301 confirmed coronavirus cases in India, which includes 56 fatalities. The NHA has issued a warning to consult specific hospitals if you have any COVID-19 symptoms. There are treatment, testing, and isolation facilities at every hospital. Additionally, NHA has provided a toll-free help number: 1800-112-545 or 1075. The World Health Organization (WHO) has classified Novel Coronavirus (COVID-19) as a pandemic since it is affecting the health of people in more than 100 different countries.
Ayushman Bharat Yojana (PM-JAY) Health Benefits Packages 2.0 & Rates (Update on 11 March 2020)
The Ayushman Bharat Yojana (PM Jan Arogya Yojana) Treatment List in Health Benefits Packages 2.0 and their costs have been made public by the central government. Ayushman Bharat PMJAY’s Health Benefits Packages 2.0 have already been implemented in a number of states, including Uttar Pradesh. As a result, out of the 5 states, UP is the first to implement HBP 2.0. Prior to the completion of the new health benefits package’s pilot project in Nagaland, numerous states expressed interest in adopting it. Health Benefits Package 2.0 includes over 1578 procedures.
Diverse cross-specialty packages have been established as part of the new benefits package to reduce duplication. 237 new packages have been added to HBP 2.0, which has 554 packages that have been dropped. There are 1393 therapy packages in HBP 1.0, 1083 of which are surgical, 309 of which are medical, and 1 package that is not stated.
As a result, HBP 2.0 of the Ayushman Bharat Yojana comprises 872 treatment packages with 1,578 procedures. Among these, 260 medical packages have 526 treatments, whereas 612 surgical packages contain 1052 operations.
Health Benefits Packages under Ayushman Bharat PMJAY (2.0) and Prices
The complete list of medical professionals and their associated costs are now available to view on Ayushman Bharat-PMJAY HBP 2.0. This can be verified by going to the PMAY website (www.pmjay.gov.in) or by clicking on the following link:
https://pmjay.gov.in/sites/default/files/2020-01/HBP_2.0-For_Website_V2.pdf
Up to Rs. 5 lakh in annual health insurance coverage is offered to families through Ayushman Bharat – PMJAY. More than 10.74 crore poor and vulnerable families will receive this amount for hospitalization in secondary and tertiary care. The government would enable beneficiaries with cashless and paperless access to services at the point of service under PM Jan Arogya Yojana.
Over 20,761 public and private hospitals have been empanelled to date across the country to offer in-patient treatments to the beneficiaries. More than 88 lakh hospital admissions of Rs. 12,169 crores have been permitted under the scheme, according to the National Health Authority (NHA). The NHA is the key organization for putting the AB-PMJAY scheme into action.
51 lakh Beneficiaries of Ayushman Bharat in Bihar
Ayushman Bharat Yojana implementation in Bihar has achieved a significant milestone through March 2020. Up to 51 lakh beneficiaries of the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB PM-JAY) had already got their electronic cards. Over 24.19 lakh families have received electronic cards. These are 22% of the Pradhan Mantri Jan Arogya Yojana eligible families in the state.
Packages for Ayushman Bharat Health Benefits Added (237 HBP), Rates of 270 Increased (Update on 28 September 2019)
The Ayushman Bharat Health Benefits Packages have been updated by the National Health Authority (NHA). In the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana, NHA has included 237 new packages (AB-PMJAY). While 43 stratified health benefits packages have been adopted, the rates for 270 Health Benefits Packages (HBP) have not changed.
According to NHA, the range of treatments covered under PM Jan Arogya Yojana will not be impacted by the adjustment to the HBP packages. A drop in the rate of 57 packages and the discontinuation of about 554 packages would occur without compromising the scope of treatment covered under the AB-PMJAY scheme.
This decrease in Ayushman Bharat Health Benefits Packages would stop fraudsters at various levels from abusing the packages.
Ayushman Bharat Health Benefits Packages Revision
More private hospitals will join the PMJAY scheme as a result of the revisions made to the Ayushman Bharat Health Benefits Packages (HBP). The table below provides access to the HBP packages revision:-
| Rates After AB-HBP Revision | Number of Packages |
|---|---|
| Increase in Rates | 270 Packages |
| Adopted | 43 Packages |
| No Change | 469 Packages |
| Reduction in Rates | 57 Packages |
| Discontinued | 554 Packages |
| Newly Added | 237 Packages |
Health Benefits Packages Revision
NHA has made an effort to maintain the costs of abuse-prone packages as low as possible in order to reduce the incentives for misuse. Ayushman Bharat health coverage schemes will be revised, and several new private hospitals will be accredited under the PMJAY scheme. Through this, access to high-quality healthcare will be improved, and thousands of vulnerable families will receive free care.
The Ayushman Bharat packages
The 1,393 treatment packages offered by the PMJAY health insurance scheme are cashless and paperless. Out of these, 1,083 are surgical, 309 are medical, and one is unidentified. These AB health benefits packages cover the cost of diagnostics up to 3 days before hospitalization and medications up to 15 days after hospitalization. Feedback on different facets of the PMJAY plan, including the current HBP and their rates, is continuously provided to NHA.
Feedback from the States and Union Territories was also gathered before the revisions to the Health Benefits Packages were finalized. The Ayushman Bharat – PM Jan Arogya Yojana review committee looked at their suggestions.
All states and UTs that are putting the AB-PMJAY scheme into practise using the insurance model or a mix of the trust and insurance model will have discretion over this choice. They can either switch to the new version after making the necessary changes to their contract or they can continue executing the Ayushman Bharat Yojana utilizing the current package master until the end of their current contract period.
Ayushman Bharat HBP Revision’s Cancer Care Revamp
Beneficiaries will receive improved cancer care because of the Ayushman Bharat Scheme’s updated oncology packages. This will be in line with the country’s current best practises. With a decrease in the catastrophic costs related to cancer treatment, the updated HBP rates will further improve cancer care in the country.
Following AB-HBP revision, oncology packages have been divided into numerous surgical, medicinal, and radiation therapy regimens. As a result, the definitions and terminology of packages will be standardized. NHA has begun the process of aligning HBP with the International Classification of Health Interventions (ICHI) and International Classification of Diseases (ICD) coding of the WHO in conjunction with the World Health Organization (WHO). India would be the first nation to use ICHI on the HBP list once it is finished.
Addressing Price Movement in the Ayushman Bharat Scheme
The pricing of implants and high-end consumables will also be configured independently at the backend of NHA’s IT system. This would be helpful in the event that the cost of these important package-related components changes.
Download the PM Jan Arogya Yojana app for the Ayushman Bharat (PM-JAY) scheme. (Update: February 8, 2019)
For smartphone users, the Ayushman Bharat Scheme or Pradhan Mantri Jan Arogya Yojana mobile application has been launched by the central government. The Ayushman Bharat – PM Jan Arogya Yojana (AB-PMJAY) app is now available for download by everyone from the Google Play store. The 4.52 MB Ayushman Bharat (PM-JAY) mobile app was created by the National Health Authority and is now accessible to Android users only.
The Modi government’s flagship yojana, PM-JAY, aims to offer cashless secondary and tertiary care from accredited public and private hospitals. More than 10 crore poor and vulnerable beneficiary families are covered by the AB-PMJAY scheme.
Download the Ayushman Bharat (PM-JAY) mobile app
The state government has allotted Rs. 6400 crores for the Ayushman Bharat – PM Jan Arogya Yojana, a mega health insurance scheme, in the most recent Union Budget 2019–20. The National Health Authority (NHA) is the supreme body in charge of putting Ayushman Bharat PM-JAY into action. NHA has now created the Ayushman Bharat (PM-JAY) mobile app, which Android users can download from Google Play. Here is the official website link to download the Ayushman Bharat mobile app. Installing the Jan Arogya Yojana app
This Ayushman Bharat Scheme PM-JAY mobile app allows users to check their wallets. The amount of money that has been spent will be shown on this AB-PMJAY app, and users can also submit complaints here. The central government estimates that the number of downloads for this PM Jan Arogya Yojana mobile app, which has been in testing for the past few days, will exceed one lakh. It has already had 10,460 downloads.
On September 23, 2018, PM Narendra Modi announced the Ayushman Bharat Yojana, starting in Jharkhand. With the help of a network of Empanelled Health Care Providers, the PM Jan Arogya Yojana will benefit approximately 55 crore individuals and offer Rs. 5 lakh for hospitalization in secondary and tertiary care (EHCP).
PM Jan Arogya Yojana Facts (AB-PMJAY)
10.33 lakh beneficiaries have been admitted to hospitals, and claims totaling Rs. 1041.3 crores have been resolved as of this writing, of which about Rs. 808.2 crores have already been approved. In addition, out of the 60,328 hospitals that applied for empanelment, 14,434 (24.4%) have received it as of right now. The government has also produced an additional 4.63 lakh cards, bringing the total to 1.28 crore.
IBEF estimates that the Indian healthcare market as a whole is currently worth $100 billion and will reach $280 billion by 2020, increasing at a CAGR of 22.9%. Visit pmjay.gov.in to see the official website for additional information.
Benefits of the PM Jan Arogya Yojana App for Ayushman Bharat (AB-PMJAY App)
The Ayushman Bharat (PM-JAY) app would also address the problem of an increase in fraudulent apps that entice smartphone users to pay by making misleading claims about membership in the PM Jan Arogya Scheme. People would have access to all PM Jan Arogya Yojana-related information. Additionally, it is simple for people to check their eligibility and even look up accredited hospitals.
After the release of the AB-PMJAY mobile app, Google has assured that the app will now rank at the top of the list thanks to search engine optimization. There are now about 28 states and union territories participating in the scheme.
How to Get a Job as an Ayushman Bharat Arogya Mitra: Eligibility & Details (Update on 26 November 2018)
Ayushman Bharat Yojana was launched by the central government and has given around 1,000,000 Arogya Mitras jobs in hospitals with empanelled status. Finding Arogya Mitra Ayushman Bharat jobs – PM The most often asked question nowadays is about the massive Jan Arogya Yojana (AB-PMJAY) health insurance scheme. People can review the requirements, the application process, and the instructions for the Ayushman Mitra position with a salary of Rs. 15,000 at the hospitals that have been granted empaneled status.
The Ayushman Bharat scheme seeks to give everyone in India a long life because Ayushman means “long life.” People can receive cashless and paperless medical care in any public or private hospital that has been accredited thanks to the Ayushman Bharat Yojana. With this scheme, 50 crore poor individuals will receive Rs. 5 lakh in health insurance for secondary and tertiary hospitalization. Arogya Mitras are crucial to the success of the Ayushman Bharat Yojana.
Now review the Arogya Mitras eligibility requirements, job duties, pay scale, hiring procedure, and other information in this post.
Job / Salary for Ayushman Bharat Arogya Mitra
Beneficiaries can check their names, visit any hospital that has been approved by PMJAY, and verify their identity using just one form of identification (such as a ration card, voter card, ayushman family card, or aadhaar card) while receiving cashless care. People can meet the individual at the Arogya Mitra-named help desk after visiting the hospitals. These Arogya Mitras are carefully selected individuals who are present in all hospitals with empanelled status to help patients receive cashless and paperless care. These employees assist people with the claim settlement process and are fully knowledgeable about the Ayushman Bharat Yojana, treatment protocols, and package prices.
The central government put a lot of effort into creating a system of assistance for beneficiaries at Empanelled Health Care Providers while introducing the scheme (EHCP). Arogya Mitra has been stationed at each EHCP in order to streamline the entire process of providing healthcare and give beneficiaries of the Ayushman Bharat Yojana a smooth experience. We must inform you that anyone interested in working as an Arogya Mitra with a salary of Rs. 15,000 can get in touch with the hospitals that have been granted empanelled status through the Ayushman Bharat Scheme directly.
Criteria for Arogya Mitra’s Eligibility
A certified frontline health service professional known as an Arogya Mitra or Ayushman Mitra (AM) must be present at each EHCP and act as the beneficiaries’ initial point of contact. The entire list of requirements to be chosen as an Arogya Mitra is shown below: –
- He or she must have graduated with a 12th grade (10+2) from an accredited institution.
- Candidate must be capable of performing simple computer tasks.
- Must have successfully finished the Ayushman Mitra Training Course and earned the required certification.
- Candidates must be able to communicate effectively in Hindi, English, and the state or region’s native tongue.
- The applicant must have sufficient functional computer literacy, including knowledge of the Microsoft Office Suite and internet portal navigation.
For the position of Ayushman Mitra, the central government has introduced a clause that gives preference to female candidates. Preference for the post of AM may be granted to all eligible ASHA employees. The state government may also designate members of the current staff of public hospitals to serve as Ayushman Mitras.
Who will conduct the recruitment process for the Ayushman Bharat Arogya Mitra position?
Here, we’ll provide you with details about the agencies responsible for organizing the Arogya Mitras recruiting drive:
- The State Health Agency (SHA) is free to recruit Arogya Mitra using any method for public facilities, including third-party agencies. The Ayushman Mitras’ salary will be paid by the SHA through third-party agencies. If more AMs are hired, SHA or the chosen agency will be able to scale up its capacity and deliver the required number of AMs.
- At the state/district or hospital level, SHA has the authority to hire AMs directly.
- The present personnel of public hospitals may also be proposed as AMs by the state government in the event that more AMs are needed.
- The hiring and placement of Arogya Mitra would be handled by the healthcare provider itself for private EHCP. AM expenses in such a facility will be the responsibility of the private EHCP.
Every public EHCP will have AMs assigned, and the precise number of AMs will be based on the number of cases that are typically handled in a given day. In the event that there are between 0 and 10 cases, 1 AM will be necessary. Two AMs would be needed for instances involving 10 to 20 people in a single day, three AMs for cases involving 20 to 30, and four AMs for cases involving more than 30 people. On the basis of performance, Arogya Mitra’s contract may be renewed annually beyond the original one-year period.
Guidelines for Hiring Arogya Mitra
All Arogya Mitras can view the responsibilities to be carried out at the assistance desk or kiosk, information about the training, and other advantages for Ayushman Mitras. Please click the following link to view the Arogya Mitra hiring guidelines: –
Guidelines for Ayushman Mitras
Before submitting an application for this position, all applicants must meet the requirements listed below.
List of Specialties and Specialty Treatment Codes Covered by PMJAY (10 Nov 2018)
The central government immediately following the launch of the schemes issued the list of specialties covered and specialty codes under the Pradhan Mantri Jan Arogya Yojana (PMJAY). At pmjay.gov.in or mera.pmjay.gov.in, the official website, you may view the full details of the specialties codes and their names. Specialties are displayed as S & M codes in the list of hospitals that have been accredited by the Ayushman Bharat health insurance scheme.
All PM Jan Arogya Yojana beneficiaries can use these specialty codes to find out which specialties are covered at any hospital that has been accepted into the scheme. Beneficiaries of the PMJAY can choose the finest hospital nearby according on their needs after gaining access to the covered specialties. The 24 specializations that fall under the purview of PMJAY are divided into 8 M codes and 16 S codes.
The PMJAY list of accredited hospitals includes the specialty codes in the far right column along with information about the facility, including type, location, e-mail address, and phone number. Here is a list of every specialty covered by the Ayushman Bharat health insurance scheme, together with the specialty codes assigned to each specialty:
PMJAY Specialty List & Codes
| S. No. | Name of Specialty | Specialty Code |
|---|---|---|
| 1. | General Medicine | M1 |
| 2. | Pediatric medical management | M2 |
| 3. | Neo-natal | M3 |
| 4. | Pediatric cancer | M4 |
| 5. | Medical oncology | M5 |
| 6. | Radiation oncology | M6 |
| 7. | Emergency room packages (care requiring less than 12 hrs stay) | M7 |
| 8. | Mental disorders package | M8 |
| 9. | General surgery | S1 |
| 10. | Otorhinolaryngology | S2 |
| 11. | Ophthalmology | S3 |
| 12. | Obstetrics & gynaecology | S4 |
| 13. | Orthopedics | S5 |
| 14. | Polytrauma | S6 |
| 15. | Urology | S7 |
| 16. | Neurosurgery | S8 |
| 17. | Interventional neuroradiology | S9 |
| 18. | Plastic and Reconstructive | S10 |
| 19. | Burns management | S11 |
| 20. | Cardiology | S12 |
| 21. | Cardio-thoracic & Vascular Surgery | S13 |
| 22. | Pediatric surgery | S14 |
| 23. | Surgical oncology | S15 |
| 24. | Oral and maxillofacial surgery | S16 |
According to the names of the specialties, M specialty codes are numbered from 1 to 8 (M1 to M8), whereas S specialty codes are numbered from 1 to 16 (S1 to S16).
Ayushman Bharat – PM Jan Arogya Yojana (AB-PMJAY) Hospital List (Update on 9 November 2018)
The central government has published the list of hospitals for the Ayushman Bharat (Pradhan Mantri Jan Arogya Yojana – PMJAY) scheme. On the official website at pmjay.gov.in or mera.pmjay.gov.in, you can see the complete list of hospitals that have been approved to participate in the Ayushman Bharat – PM Jan Arogya Yojana. The names and contact information of hospitals where eligible Ayushman Bharat Yojana participants can receive treatment are listed on this website.
The 50 crore persons covered by the PMJAY national health protection scheme are eligible to receive treatment in any government- or privately-empanelled institution. These hospitals would provide cashless and paperless care at NHPM treatment package costs. Arogya Mitras are available at every hospital to help patients easily settle their PMJAY claims.
Anyone whose name appears on the list of PM Jan Arogya Yojana participants is eligible to receive care anywhere in India through the AB-NHPM scheme in any hospital that has been approved by doing nothing more than displaying their Ayushman family card, ration card, voter card, or Aadhaar card.
Hospitals in Ayushman Bharat are listed at abhnpm.gov.in
The complete process to verify the name, address, and contact information of Ayushman Bharat hospitals included in the Pradhan Mantri Jan Arogya Yojana list of accredited hospitals is described below:
Step 1: Visit the official website first at www.pmjay.gov.in.
Step 2: On the homepage, click the main menu item labeled “List of Empanelled Hospitals” or just click this link.
Step 3: The next moment, the hospital’s search page will open as depicted in the image below:
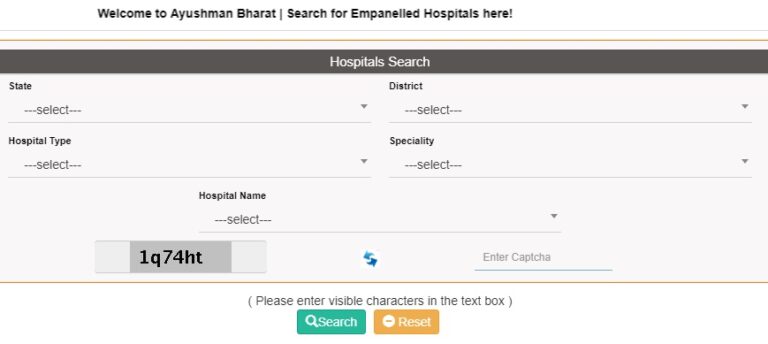 PM Jan Arogya Yojana Hospital List
PM Jan Arogya Yojana Hospital List
Step 4: Choose the district, state, kind of hospital, specialty, and name of the hospital, then click “Search” to get a list of all hospitals that have been given empaneled status in that location.
Step 5: Simply select the state and/or district you want to view and click the “Search” button if you want to see the entire list of states or districts. A sample of the full list of hospitals in the Haryana district of Faridabad is provided in the graphic below:
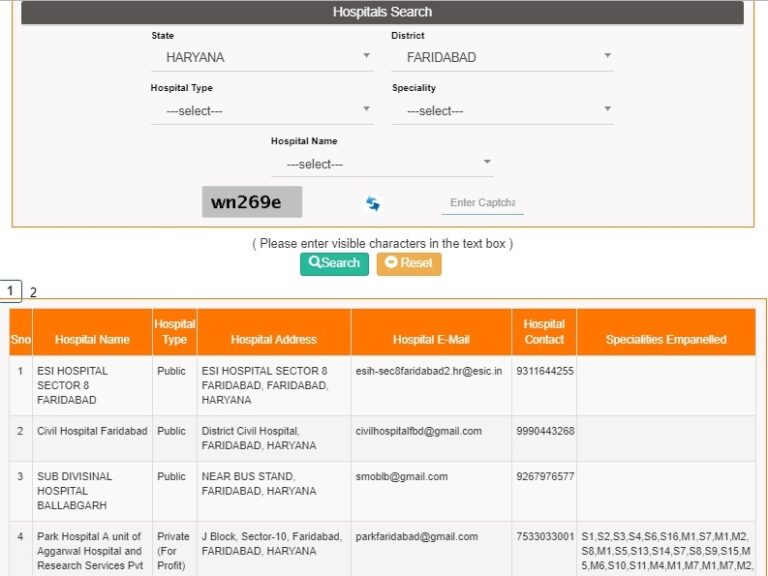 List of Ayushman Bharat Hospitals
List of Ayushman Bharat Hospitals
Step 6: PMJAY participants can check the kind of hospital, address, email address, phone number, and specialisations offered at different hospitals in this list.
Visit mera.pmjay.gov.in to view the Ayushman Bharat Yojana Hospitals List.
You can also examine the list of hospitals that have been approved to enroll in the PM Jan Arogya Yojana at mera.pmjay.gov.in, where the following method is described:
Step 1 – Visit the PMJAY “Am I Eligible Portal” at mera.pmjay.gov.in as the first step.
Step 2 – Click the “Search Hospitals” link on the site, which is located on the main menu, or just click this link.
Step 3 – From Step 3 through Step 6, the process is the same as what was described earlier. Check the Ayushman Bharat Yojana hospitals list using the same process.
Under this PM Jan Arogya Yojana, approximately 1354 medical examinations and operations are covered (PMJAY). One need only looks up their name on the Ayushman Bharat Yojana recipients list. To receive cashless treatment in any of the above empaneled hospitals, beneficiaries must meet the PMJAY eligibility requirements and present one of the acceptable forms of identification. The Pradhan Mantri Jan Arogya Yojana details are available to all beneficiaries, who can use them to learn more about this comprehensive health insurance scheme.
Aadhaar is mandatory under the Ayushman Bharat Yojana (PMJAY) for second-time treatments (Update on 8 October 2018)
The Aadhaar card is now required for anyone seeking treatment under the PMJAY scheme for the second time, even though it was previously optional to receive benefits under the Ayushman Bharat – PM Jan Arogya Yojana (AB-PMJAY). This ruling follows the Supreme Court’s (SC) declaration that Aadhaar is a valid constitutional document. Since the Aadhaar card is now a recognized identity document, the government has made it a requirement for second-time treatment under the Ayushman Bharat Yojana.
Beneficiaries of the Pradhan Mantri Jan Arogya Yojana do not need to worry if they do not have an Aadhaar number. Such AB-PMJAY beneficiaries only need to show proof of enrollment in order to receive a 12-digit unique identification number. This choice will assure that everyone receives the advantages of the massive National Health Protection Scheme (NHPS) and that only eligible beneficiaries do so. This choice is in agreement with the National Health Agency’s notice, which is in charge of carrying out the Ayushman Bharat-PM Jan Arogya Yojana.
Aadhaar Required for Second Treatment Under Ayushman Bharat (PMJAY)
The Aadhaar number is now required by the Central Government in order to receive the benefits of health insurance under the AB-NHPM scheme for a second time. According to the official statement, “We are analyzing the Supreme Court judgment. To receive treatment under the scheme for a second time, you must present your Aadhaar number or, at the very least, documents proving that you registered for the 12-digit unique identifying number. To use the Pradhan Mantri Jan Arogya Yojana plan advantages, one must first present their aadhaar card, voter card, ration card, or golden card.
The Prime Minister started the Ayushman Bharat-National Health Protection Mission (AB-NHPM), now known as AB-PMJAY, across all of India on September 23, 2018, starting in Jharkhand. The largest health insurance scheme in the world, PM Jan Arogya Yojana, has benefited around 47,000 people to date. Additionally, about 92,000 individuals have already received golden cards that allow them to receive care at NHPM package rates in government- and privately-run empaneled institutions.
There are no limitations on family size, age, or gender under the AB-PMJAY scheme, which will help 10.74 crore underprivileged households. Through a network of Empanelled Health Care Providers, the government hopes to offer Rs. 5 lakh per family per year for secondary and tertiary hospitalization through this Ayushman Bharat Yojana (EHCP).
 Aadhaar Mandatory Second-Time Treatment Ayushman Bharat Scheme
Aadhaar Mandatory Second-Time Treatment Ayushman Bharat Scheme
At the moment of service, the beneficiary will have access to services without cash or paper. Only deprivation, not caste, religion, or community, is used to determine who would receive benefits under the Ayushman Bharat scheme. According to data from the Socio-Economic Caste Census (SECC) 2011, this NHPS scheme serves 8.03 crore people in rural areas and 2.33 crore people in urban areas.
According to NHA officials, 98% of all recipients have been located. To receive benefits from the PM Jan Arogya Yojana, people can also check the list of beneficiaries for their names. The Ayushman Bharat health insurance scheme has empanelled almost 14,000 hospitals nationwide. A total of 32 states and union territories have signed memorandums of understanding with the center to carry out this scheme. For the execution of this scheme, MoUs have still not been signed by Telangana, Odisha, Delhi, or Kerala.
Child cancer treatment is now covered by PMJAY (11 September 2018)
As of right now, the Pradhan Mantri Jan Arogya Yojana will pay for the treatment of child cancer. The government has already set the prices for paediatric care, according to NITI Aayog member Dr. Vinod Kumar Paul. According to Dr. Paul, the scheme will offer low-income households a five lakh rupee health insurance policy. BPL and lower middle class families, according to him, will profit from it. As part of the Ayushman Bharat Scheme, the Union government has agreed to launch 1.5 lakh Health and Wellness Centers by FY 2022. These HWCs will provide complete medical care for conditions like diabetes, cancer, hypertension, and cardiovascular illnesses.
A official of NITI Aayog stated that the Pradhan Mantri Jan Arogya Yojana will provide access to therapy for children with cancer (PMJAY). On September 9, 2018, Vinod Kumar Paul disclosed this information while at a gathering in New Delhi. 1350 diseases have treatment package pricing approved by the central government. The PM Jan Arogya Yojana will also cover the treatment of children cancer in addition to these illnesses. The following factors make it necessary to include childhood cancer in the AB-PMJAY Scheme:
- Childhood cancer is a treatable disease if discovered in its early stages.
- This illness does not transmit from one child to another and is not infectious.
- Typically, genes are not the cause of childhood cancer. For a high cure rate, early diagnosis and timely treatment are essential.
- Cancer in children is very different from cancer in adults. Children grow quickly, but they are extremely sensitive to chemotherapy. They have a chance to recover quickly, making cancer therapy a feasible and attainable objective.
- To maintain treatment discipline and regularity, proper hygiene, and balanced nourishment, extra care should be made of children at home.
- It is recommended that children receive treatment in a knowledgeable and specialist paediatric cancer unit because cancer therapy is a demanding process.
Around 3% of children have cancer, which is remarkably low. The cure rate is high, and even the overall number of years of productive life spared after healing children is high. Thus, the government intends to include paediatric cancer treatment in the PM Jan Arogya Yojana (PMJAY).
Ayushman Bharat Scheme Announces Pradhan Mantri Jan Arogya Abhiyan (Update on 15 August 2018)
On the occasion of the 72nd celebration of Independence Day, PM Narendra Modi declared the beginning of the Pradhan Mantri Jan Arogya Abhiyan. Before the 2019 Lok Sabha elections, PM Modi will make one final speech. On September 23, 2018, the Ayushman Bharat Scheme will introduce PM Jan Aarogya Abhiyan. Around 50 crore people would receive Rs. 5 Lakh in health insurance as part of the Ayushman Bharat – National Health Protection Mission (AB-NHPM), which will promote access to affordable healthcare.
From the Red Fort in New Delhi, Prime Minister Narendra Modi is currently addressing the country. It is Prime Minister Modi’s fifth and last speech on July 4. Recently, the prime minister asked for suggestions from the public for his Independence Day speech. The Jan Arogya Yojana software will undergo testing over the next six to seven weeks, and this scheme will finally be introduced on Pt. Deendayal Upadhyaya’s birthday (25 September).
Announcement for the Pradhan Mantri Jan Arogya Abhiyan
On the day of India’s 72nd Independence Day celebration, Prime Minister Modi announced the launch of the Pradhan Mantri Jan Arogya Abhiyan. This National Health Protection Scheme will produce reasonable individuals access to affordable healthcare facilities. The central government will put this initiative into action using technology and software to ensure transparency.
The testing process of this software is currently underway and will last for the next six to seven weeks. This cashless and paperless treatment facility will then be accessible to about 50 crore people. The Pradhan Mantri Rashtriya Swasthya Suraksha Mission will then provide health insurance to all families for a total of Rs. 5 lakh per year (PMRSSM). All those whose names appear on the rural and urban Ayushman Bharat Yojana Yojana list may receive treatment under the Pradhan Mantri Jan Aarogyaan at NHPM Treatment Package Rates.
Guidelines for Claim Settlement have been made public for the Pradhan Mantri Jan Arogya Abhiyan. All Health and Wellness Centers, public hospitals, and privately empanelled hospitals accept claims from patients. In order to help people and support them during their treatments, Ayushman Mitras will be hired. Beneficiaries will receive Ayushman Family Cards in order to access treatment benefits.
The PMJAY (Pradhan Mantri Jan Arogya Yojana) logo
On August 27, 2018, the Pradhan Mantri Jan Arogya Yojana (PMJAY) logo for Ayushman Bharat was unveiled. The following figure shows it:
 Pradhan Mantri Jan Arogya Yojana PMJAY Logo
Pradhan Mantri Jan Arogya Yojana PMJAY Logo
Beneficiaries of the Ayushman Bharat Yojana must register at Common Service Centers (CSCs) (Update on 1 August 2018)
An MoU was signed between the Common Service Center (CSC) and the National Health Accounts (NHA) to implement the Ayushman Bharat Yojana through 3 lakh CSCs. CSC Initiative on Telemedicine will receive funding from the health ministry. In India, CSCs can now register Ayushman Bharat beneficiaries. The National Health Protection Scheme will give coverage for secondary and tertiary care hospitalization up to Rs. 5 lakh per household per year for 50 crore poor people.
The Ayushman Bharat Yojana beneficiaries’ identification and registration would be handled via CSCs. The MoU was signed in front of Shri JP Nadda, Minister of Health and Family Welfare, and Shri Ravi Shankar Prasad, Minister of Electronics and IT. The largest healthcare system in the world, the AB-NHPM, is currently choosing CSCs for adoption. In rural India, CSCs have emerged as a key tool for change.
Ayushman Bharat Beneficiaries Register at CSC Centers for Benefits
By registering at CSCs, all Ayushman Bharat beneficiaries can receive the following benefits:-
- The Ayushman Bharat Scheme will now be implemented through CSC centers thanks to MoH&FW and CSC SPV.
- Any Beneficiary may visit a CSC that is close by to receive benefits from this scheme.
- Beneficiaries of Ayushman Bharat will receive assistance from CSCs in locating their names in the MoH&FW database and determining their eligibility for this scheme.
- Additionally, CSCs will assist beneficiaries in scanning and uploading their KYC documents in order to verify their identity and claim their benefits.
- Through CSC Centers, beneficiaries can even print their Ayushman Family Cards. Their source claim will be based on this.
- To make sure that the greatest number of beneficiaries can make use of this benefit, CSCs will raise awareness of the Ayushman Bharat Scheme and encourage its use among citizens.
For assistance with beneficiary identification, document upload, and laminated card printing, CSCs will receive Rs. 30 (tax included).
Beneficiaries of Ayushman Bharat must register through CSCs: Process
The procedure that any Ayushman Bharat beneficiary must follow at CSCs is listed below:
- All beneficiaries must visit a nearby CSC center to verify their Ayushman Bharat Yojana eligibility.
- Then, the CSC Center will determine if the beneficiary is eligible for NHPS. The required information and documents, including Aadhaar Cards, Ration Cards, PAN Numbers, and others, will be uploaded by CSC VLEs.
- The CSC Center will now forward the information regarding new applicants for approval to the relevant approver / state authority for additional approval and verification.
- SLA has been hired by MoH&FW to get this application accepted within certain timeframes and to respond to it in real time (RTS).
- The Ayushman Beneficiaries will subsequently receive a printed card on paper from CSC Center.
- Each beneficiary can use these cards at hospitals that have been approved by the Ayushman Bharat Abhiyan to submit claims for benefits.
The Common Service Centers (CSCs) will alter the course of events in our country. Then, at the NHPM Portal, patients can receive care at predetermined Package Rates.
Common Service Centers’ (CSCs’) role in PMRSSM
Common Service Centers (CSCs) have always been crucial in transforming rural residents’ quality of life. Through Stree Swabhiman, these CSCs have significantly improved menstrual hygiene. With the addition of CSCs, the Ayushman Bharat Yojana is helping the dream of a digital India take a giant step forward.
A innovative universal healthcare scheme will help 10 crore families in India through the PM Rashtriya Swasthya Suraksha Mission (PMRSSM). In 2.5 lakh Panchayat, there are about 3 lakh CSCs, which would be quite helpful in putting this scheme into action. Under the Digital India Initiative, these CSCs will play a significant role in developing a new economic paradigm for rural populations.
One Lakh Ayushman Mitra Jobs in Hospitals With the PMRSSM Empanelment – Rs. 15,000 Salary (Update on 28 July 2018)
Under the Pradhan Mantri Rashtriya Swasthya Suraksha Mission, the central government plans to directly deploy 1 lakh, Ayushman Mitra, in public and private hospitals (PMRSSM). The National Health Protection Mission known as Ayushman Bharat is expected to generate a total of 10 lakh jobs (AB-NHPM). All young people engaged through the Ayushman Bharat Yojana would receive a salary of Rs. 15,000 per month.
Ayushman Bharat Yojana will produce a number of openings for the positions of doctors, nurses, staff, technicians, and other positions. In the current fiscal year 2018, about 20,000 Ayushman Mitra will be deployed.
The Health Ministry and the Skill Development Ministry have reached an agreement about this hiring. Currently, the government is trying to appoint 20,000 hospitals to the National Health Protection Scheme (NHPS). Additionally, Ayushman Mitra will be given a bonus of Rs. 50 for each beneficiary.
Mitra Ayushman Works under PMRSSM
Under the Ayushman Bharat Yojana, each Ayushman Mitra will be required to complete the following tasks:-
- Ayushman Mitras will need to learn everything there is to know about the Ayushman Bharat Portal.
- They will need to put some effort into the software being developed for patient welfare.
- Employing QR codes to confirm the chosen beneficiaries’ identities (ID).
- To give information on the hospital where patients will receive their treatment.
- After the patient is discharged, tell the state agencies of the beneficiary’s present situation.
 Rashtriya Swasthya Suraksha Mission Ayushman Mitra PMRSSM
Rashtriya Swasthya Suraksha Mission Ayushman Mitra PMRSSM
All hired applicants will be required to complete duties involving the well-being of beneficiaries.
Schedule for Ayushman Mitra’s training
All Ayushman Mitra will receive training from the government, which will start in August 2018. The government will choose one trainee for this purpose from each district and will give them the appropriate training. These students will next receive instruction at the Pradhan Mantri Skill Development Centers (Kaushal Vikas Kendras).
The Ministry of Health will then administer the test, and each candidate who passes will receive a certificate. Every person who has a certificate will become an Ayushman Mitra. These chosen individuals will then be sent out in accordance with the requirements of the state. A 50 rupee reward will also be given to each beneficiary.
11 Cr Ayushman Family Cards under PMRSSM for Health Insurance (Update on 18 July 2018)
The Pradhan Mantri Rashtriya Swasthya Suraksha Mission will see the print and hand-delivery of 11 crores “Ayushman Family Cards” (PMRSSM). To make use of the flagship Ayushman Bharat Yojana’s cashless treatment benefits, these cards are required (Modicare). To provide Health Insurance Scheme advantages to the underprivileged rural population, Ayushman Pakhwaras would be set up throughout the villages.
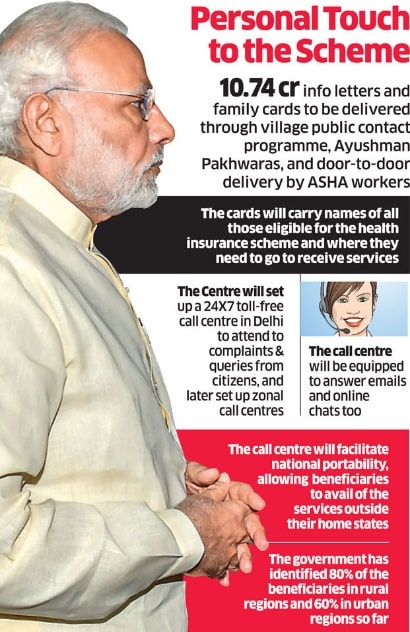
The Ayushman Bharat Yojana Beneficiaries will even receive a new National Toll-Free Number. Call Centers will be available 24/7 to handle concerns about Ayushman Bharat Yojana applications and National Health Protection Scheme claim settlement. The Modi Government has previously published the Treatment Package Rates, and Ayushman Family Cards are required to receive treatment at these rates as well as other HWC Services. With 50 crore beneficiaries, this scheme will assist 10 crores, of vulnerable families. Beneficiaries of Ayushman Bharat can now register at Common Service Centers (CSCs).
- The government expects to finish all of the preparations by August 15th, 2018, however, the launch date is yet unknown. The central government will establish a 24-hour call center in the nation’s capital to handle citizen complaints and questions about the scheme. Even if they are outside of their native state, beneficiaries will still receive support. The following are the key characteristics of these Modicare Ayushman Family Cards:-
- The identities of every member who qualifies for this Ayushman Bharat Yojana will be listed on every Ayushman Family Card.
- These Ayushman Cards will also come with a customized letter outlining the characteristics of the Pradhan Mantri Rashtriya Swasthya Suraksha Mission (PMRSSM).
- Approximately 80% of the beneficiaries are in rural areas, and 60% are in urban areas, according to data from the central government.
- For such a massive Health Insurance Scheme, a National Toll-Free Number will be required to contact the Call Center.
- All parties involved will be able to obtain information and services easily and quickly thanks to these call centers. Additionally, in these centers a family does not have one of these family health cards, treatment benefits will still be provided to that family. will have the capability of responding to online chats and emails from users.
- Ayushman Family Cards will aid in beneficiary identification, and further documents will be needed to verify the data.
- Over the following two years, the government intends to hand distribute around 107 million informational letters and family cards to the populace.
 Health Card Ayushman Bharat Yojana
Health Card Ayushman Bharat Yojana
People will be less apprehensive about their eligibility for the PM Rashtriya Swasthya Suraksha Mission thanks to Ayushman Family Cards (Modicare).
Distribution of Ayushman Bharat Yojana Health Cards
The service providers will print these Ayushman Family Cards after receiving beneficiary data from the National Health Agency. Under the Modicare Scheme, all Health Cards will adhere to the Data Safety Standards and Right to Privacy. After that, service providers will group these cards according to area codes before sending them to the district headquarters of the recipients. Through significant public outreach initiatives, these Health Cards would then be distributed to the Gram Panchayats and ultimately to underprivileged families.
Health professionals will conduct mass gatherings similar to Ayushman Pakhwaras in villages and door-to-door. The Hub-and-Spoke Model will be used by call center service providers to set up zonal call centers around the nation. Call centers will also help this PM Rashtriya Swasthya Suraksha Mission’s National Portability Advantage (PMRSSM). The government will be able to serve the public effectively and efficiently because of these call centers’ geo-tagging capabilities. The calls will subsequently be classified according to their locations and directed to the closest call center.
Visit pmjay.gov.in to view the Ayushman Bharat Yojana (PMRSSM) Claim Settlement Guidelines (Update on 12 July 2018)
The Ayushman Bharat Yojana/Pradhan Mantri Rashtriya Swasthya Suraksha Mission claim settlement procedures have been made public by the central government (PMRSSM). All Empanelled Health Care Providers (EHCP) shall manage transactions relating to claims using an IT system called PMRSSM. Paperless claim registration, notification, payment, and inquiry by EHCP or by Trust/Insurer are all parts of the procedure.
The PMRSSM IT system will support online transactions to assure real-time claim reporting. However, some districts struggle with internet connectivity, therefore the government built an offline setup into this IT system. The PM Rashtriya Swasthya Suraksha Mission does away with the need to provide actual paper.
All claim data will be electronically transmitted to the Central / State server via IT system. Only their respective transaction data for the NHA, SHA, Insurer (if applicable), and EHCP shall be accessible via this data.
Claim Payment and Turnaround Time for the Ayushman Bharat Yojana
The following rules for claim settlement that Trust / Insurance Companies obtained from EHCP must be followed whenever a consumer raises a claim (has hit Central / State Server) under this PM Yojana:
–

